As Benjamin Franklin rightly said: “In this world, nothing is certain except death and taxes.” The difference is we know the date for paying taxes, but not the day our Maker will call us to account for how we have lived. Even so, both days will go better with proper planning. Just as it’s advisable to file an accurate and timely tax return, the process of dying can be ameliorated with an advance directive, known in some parts as a living will—a legal document that explains how you want medical decisions about you to be made if you are unable to make the decisions yourself.
Want to subscribe to receive blog updates sign up today!
Now that April 15th is taken care of (unless you’re like me and filed a request for an extension), April 16th is the national day set aside annually to address healthcare decisions. The goal is to (1) encourage and empower people to begin or continue conversations about their wishes for care through the end of life, and (2) educate people on the importance of advance care planning. Unlike missing a tax deadline, there’s no penalty if you don’t take action on April 16th, but there’s a clear advantage to observing the day so that healthcare professionals respect and meet your wishes.
Notably, healthcare decisions involve more than end-of-life issues. Anytime a person is incapable of making sound decisions an advance directive is critical for choosing care that matches the choice a person would make for themselves. When a person is unconscious, medical professionals often turn to next of kin to make treatment decisions on issues such as mental health, blood transfusions, and amputations, to name a few.
According to a 2018 National Survey by the Conversation Project®, 92% of Americans say it’s important to discuss their wishes for end-of-life care, but only 32% have had such a conversation. Dr. Susan Nelson suggests that “our delay in having these conversations is because it often seems too early, then, suddenly, we find it is too late.” The Conversation Project® promotes the kitchen table as the place to begin such conversations, not the ICU.
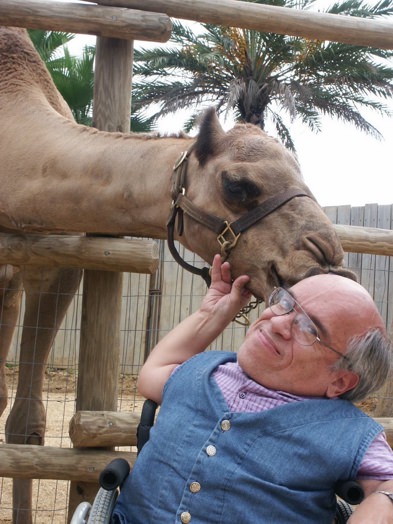
I recently found myself in this position when my husband Robert was struggling to breathe in a hospital Intensive Care Unit (ICU). I was asked to give consent for him to be connected to a ventilator to avoid his lungs from collapsing and then to begin dialysis treatment to clear the fluid from his lungs that his chronic kidney disease was preventing. I hated to make either decision because of the risk and skill needed to successfully intubate someone with his type of dwarfism—Spondyloepiphyseal Dysplasia—and the life sentence to dialysis treatment.
Yet despite my reluctance to make these decisions for Robert, I knew what choices he would make. Thankfully, we had not only had the conversation about our end-of-life care but also had taken the next critical step of formally documenting our decisions with an estate attorney. Robert appointed me as his Health Care Surrogate and signed a Living Will.
So how far along are you with advance care planning?
For useful resources go to:
- National Healthcare Decisions Day. https://nationaltoday.com/national-healthcare-decisions-day/
- Erica Costello. “National Health-Care Decisions Day.” March 28, 2024. https://www.americanbar.org/groups/law_aging/publications/bifocal/vol45/vol44issue5/nationalhcdecday/
- Susan Nelson, MD. “National Healthcare Decisions Day 2024: What You Should Know.” March 4, 2024. https://blog.ochsner.org/articles/national-healthcare-decisions-day
- “10 Ideas of Things to Do for National Healthcare Decisions Day (in 10 Minutes or Less).” Posted on 04/07/2022. https://theconversationproject.org/tcp-blog/10-ideas-of-things-to-do-for-national-healthcare-decisions-day-in-10-minutes-or-less/
- Conversation Starter Guide. https://theconversationproject.org/wp-content/uploads/2020/12/ConversationStarterGuide.pdf